Hashtag-2020 got off to a heck of a start. We thought 2019 was crazy and it would all be over with after December 31, then it even got worse. It seemed like every single day of 2020 there was some world event we never imagined. Earlier this year I tried to keep a file of the crazy headlines that popped up every day, at some point I gave up.
This is what I had so far, does anyone remember any of this by now?
Dec 31 - Pope slaps woman's hand
Jan 1 - New Years, Dustin Parker shot in OK
Jan 2 - ?
Jan 3 - Soleimani drone strike
Jan 4 - ?
Jan 5 - Iran backs out of nuclear deal
Jan 6 - Ricky Gervais Golden Globes speech roasting most of Hollywood
Jan 7 - Iran fires missiles on Iraq/US base
Ukrainian flight shot down
Earthquake in Iran
Jan ?? - Australia is on fire
Jan 8 - Prince Harry and Megan announce leaving royals
Jan 9 - ?
Jan 10 - ?
Jan 11 - Iran admits shooting down airliner
Anti-vaxxers picketing on street corners at SAP Center in San Jose
Jan 14 - Alameda SO evicts homeless squatters in Oakland
Jan 15 - Pete DeBoer (former SJ Sharks team) goes to Vegas Golden Knights
Jan 19 - SpaceX explodes a rocket for abort test
Jan ?? - Coronavirus becomes a thing in the US
Jan 26 - Kobe Bryant helicopter crash
Feb 5 - Trump acquitted of impeachment
Feb 24 - DJIA/NASD drop off cliff due to coronavirus
Mar 6 - Required work from home at work for to weeks, until Mar 21st
SXSW in Austin cancelled by city
Mar 11 - Trump bans EU->US flights, NBA suspends season, Tom Hanks has covid
Mar 12 - NHL suspends season
Mar 15 - Restaurants in Fremont close early in anticipation of SIP orders
Mar 16 - DJIA drops 2900 pt
Bay Area "shelter in place" starts
FB poke broke (srs business),
Mandatory everyone WFH till April 7
Some restaurants pivot to take-out only
Mar 19 - Whole state under shelter-in-place
US Covid topped 10k cases
Work tentatively WFH indefinitely
My birthday home alone
Mar 20 - Kenny Rogers dies, CA allows to-go beer and drinks
Mar 27 - UK prime minister catches covid
Apr 6 - UK prime minister moved to ICU
Apr 10 - Burning Man 2020 cancelled
Apr 20 - Oil futures for May contracts go negative $30
Apr 23 - Don't inject disinfectants or bright light, y'all
Apr 24 - Finally able to buy flour at the store
Apr ?? - Possible meat shortages as processing plants close
Apr ?? - People seriously believe 5G networks transmit the virus, setting fire to 5G sites
People forget Bill Gates made his billions from Microsoft,
say he invented virus to make more money
People are dumb
Apr 30 - Finally see toilet paper on the shelves, frozen meat starting to get picked over
May 3 - Murder hornets invade WA/BC!
May 8 - Saddle Rack announces it's closing for good
May 9 - Elon threatens to close Fremont factory and move Tesla HQ
Little Richard dies at 87
May 11 - Jerry Stiller, and double-rainbow guy die
Shady Grove in Austin closes
May 18 - SF Bay Area counties start phase 2 reopening
Trump casually announces he's taking hydroxychloroquine
May 21 - Yeast finally seen on the grocery store shelf
Well, shit
May 25 - George Floyd killed by police
May 27 - SpaceX Crew Dragon launch - scrubbed
US hits 100,000 covid deaths
CDC warns of starving cannibal rats
May 28 - Boston Marathon cancelled
California tops 100,000 covid cases
May 29 - More protests and riots break out
CNN crew arrested on-air, CNN center in ATL vandalized
Monkeys steal covid-positive blood samples from lab assistant in India
May 31 Sixth day of George Floyd protests, shit's on fire yo
SJ, SF, LA, under curfew for a week
Fremont shopping centers closed (Hub, Pacific Commons)
Jun 1 All of Alameda county under curfew all week
Jun 2 BLM protests at Fremont PD HQ (two blocks from me)
Jun 6 Back to flying!
Jun 19 Alameda county allows outdoor dining
Jul 10 Alameda county closes outdoor dining, dispute with state
Jul 13 Santa Clara county allows salons to open
Jul 14 State says all salons must close, suck it businesses
Jul 15 Alameda county says outdoor dining can open again
Bunch of people on twttr get hacked
Jul ?? Confederate monuments come down
Jul 29 US COVID-19 deaths hit 150,000
Aug 1 Stanley Cup playoffs start
Aug ?? Somewhere the USPS went to shit
Aug 4 Ammonium nitrate explosion craters port at Beruit, Lebanon
Aug 14 3-judge panel upholds Duncan v Becerra opinion, mag ban struck down
Aug 15 NWS issues first ever warning for "pyrocumulonimbus cloud" - fire tornado
Freak lightning/thunderstorm hits Bay Area, sets several fires
Aug 17 Possible rolling blackouts due to lack of electricity generation (deja vu 2001)
Aug ?? Mypillow.com guy pitches Oleandrin as a covid treatment, Trump loves it (whaaaaat)
Aug 17-26 California is on fire
Aug 26 Hurricane Laura, cat 4, about to hit LA
Sep 1 Pelosi indoor haircut/mask debacle (she should've went across the Bay)
Sep 2 Alameda county allows indoor salons and barbers
Sep 8 Bay Area is deeply orange colored from high altitude smoke (orange in EB)
Sep 9 Bay Area is deeply yellow colored from high altitude smoke (orange in SF)
Fucking Blade Runner 2020
Sep 10 NFL returns
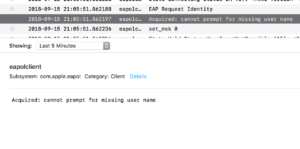
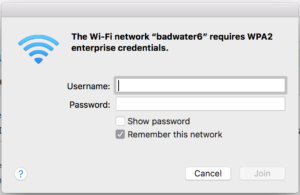
Sep 11 Finally get gigabit internet at home!
Sep 16 Hurricane Sally, cat 2, hits AL
Sep ?? Protests in Portland still going on
Sep 18 SCOTUS Justice Ruth Bader Ginsburg dies
We ran out of hurricane/tropical storm names
Sep 28 Tampa wins Stanley Cup (this should've been played in June)
Sep 22 US COVID-19 deaths hit 200,000
Oct 1 Trump says he has COVID-19
Oct 2 Trump taken to Walter Reed
Oct 4 Trump leaves Walter Reed
Oct 4-7 Everyone else in the White House and DC catch COVID-19
Oct 6 Eddie Van Halen dies
Oct 8 FBI reveals plot to kidnap/assassinate MI governor
I was able to buy Clorox Wipes for the first time since March
Oct 31 Sean Connery dies
Nov 3-4 Elections, Biden wins, crazies come out
Nov 24 Elon becomes 2nd richest person in world
DJIA hits 30,000
Nov 28 Iranian nuclear scientist is assassinated, probably Israel
Dec 1 Arecibo receiver crash
Chang'e 5 lands on moon
Dec 2 LA issues "safer at home" order
Dec 3 California issues regional shelter in place orders
Dec 6 Bay Area counties shut down again, no in/out dining, salons
Dec 11 Supreme Court shuts down Texas Trump case, says GTFO
Dec 13 First covid vaccines ship
Today is April 20 and the craziness is still going on. I still haven’t seen toilet paper in stores in weeks. I wish I had kept better track of what was available in the stores. I feel like two weeks ago I was finally able to buy bread, last week I was able to buy milk, eggs, and flour (but no yeast).
Update: Oct 9: #2020 still cooking up greatest hits!
Today people are protesting in state capitols the economy should be re-opened. People seriously still can’t figure out how air works, either you’re protecting yourself, protecting others, or both.